Hip fractures
Classified by:
- Anatomical location:
- Intracapsular- increased risk avascular necrosis
- Extracapsular
- Radiological location (garden classification):
- Higher stage- increase risk of AVN
- 1: Impacted only
- 2: Complete fracture, non-displaced
- 3: Varus displacement femoral head
- 4: Complete loss of continuity
Mechanism of injury
- Often elderly patients with osteoporosis
- Can be mild trauma, if young usually major trauma
Clinical features
- Leg- shortened and external rotated
- Unable to weight bear
Investigations
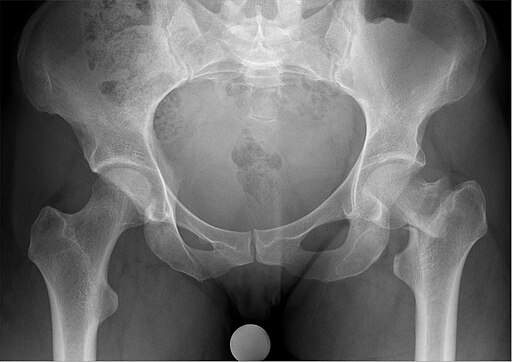
- XR- AP and lateral views
- CT or MRI if XR unclear
- Prep for theatre- bloods including G&S and cross-match, CXR, ECG
Management
- May be unwell and require resuscitation (A to E assessment, blood if needed)
- Analgesia- fascia iliaca block unless contraindication (high INR, patient refusal, on anticoagulant)
- VTE prophylaxis
- Prompt surgical intervention < 36hrs
- Options include dynamic hip screw (DHS), intrameduallary nail, hemiarthroplasty and total hip replacement (THR) depending on if intra or extracapsular and pre-morbid mobility and frailty
- Post op care joint with geriatrician
- MDT involvement for early mobilisation and discharge planning
Post operative complications
Surgical:
- Bleeding
- Surgical site infection
- Non-union
- OA
- AVN of femoral head in displaced (30% risk)
Medical:
- High mortality especially in elderly- 30% at one year even after operation
- Delirium
- Acute kidney injury
- Ileus/bowel obstruction
- VTE
- Infection most commonly chest and urine
Hip dislocation
Mechanism of injury
- Young- direct trauma i.e. road traffic accident or fall from height
- Elderly/frail- low trauma twisting/fall
Exam findings depend on type:
- Posterior= 90%
- Shortened, adducted and internally rotated limb
- Anterior
- Abducted and externally rotated
- No shortening
- Central
- Rare
Management
- Resuscitate (A to E)
- Analgesia
- Reduction under anaesthetic
- Within < 4 hrs to reduce AVN risk
- Intensive physiotherapy after
- Around 3 months for hip to heal post dislocation
Complications
- Nerve injury- femoral/sciatic
- AVN
- Osteoarthritis
- Recurrent dislocation
Femur fractures
Mechanism of injury
- High velocity injury
Examination findings
- Shortening, external rotation and abduction of limb
- May be obvious deformity
- Secondary survey- assess for other injuries- often associated with multisystem trauma
Investigation
- XR
- Trauma CT if high velocity injury
Management
- A to E and resuscitate
- Thomas splint whilst awaiting surgery
- Analgesia including femoral nerve block
- Definitive surgical management (commonly ORIF)
Knee fractures
Patella fracture
Mechanism of injury
- Direct trauma or sudden knee flexion
Examination findings
- Tender, swollen knee
- Difficulty extending knee
Management
- Analgesia
- If displaced- surgical management
- Immobilise hinged knee brace following surgery or sole treatment if surgery not indicated
Tibial plateau fracture
Mechanism of action
- Pedestrian vs car
- Fall onto extended leg
Clinical features
- Pain, swelling, bruising
Investigations
- CT to confirm fracture and for surgical planning
Management
- Elevate
- Immobilise in backslab cast
- If requires surgical management: ORIF
The Ottawa Knee Rules
The Ottawa knee rules can be used to clinically exclude a fracture and determine whether an X-ray of the knee is required. The rules dictate that knee X-ray is only required after a knee injury if there is one of the following findings:
- Age 55 years or older
- Isolated tenderness of the patella (no bone tenderness of the knee other than the patella)
- Tenderness of the head of the fibula
- Inability to flex the knee to 90°
- Inability to weight bear both immediately and during the consultation for four steps (or the inability to transfer weight twice onto each lower limb regardless of limping)
- Also, offer an X-ray of the knee if there is suspicion of a haemarthroses (i.e. large effusion within 2 hours of the injury).
