🔑 Key Learning
- Amenorrhoea is classified into primary (failure to menstruate by age 13–15) and secondary (cessation of periods for ≥3–6 months).
- Causes range from physiological (pregnancy, menopause) to endocrine (prolactinoma, PCOS, hypothyroidism) and structural (Turner’s).
- PCOS presents with oligo/amenorrhoea, hyperandrogenism, and polycystic ovaries on scan.
- Turner’s syndrome is a classic cause of primary amenorrhoea with absent secondary sexual characteristics.
- Investigations are guided by age, secondary sexual development, and hormonal profile (FSH/LH/testosterone/prolactin).
📆 The Menstrual Cycle
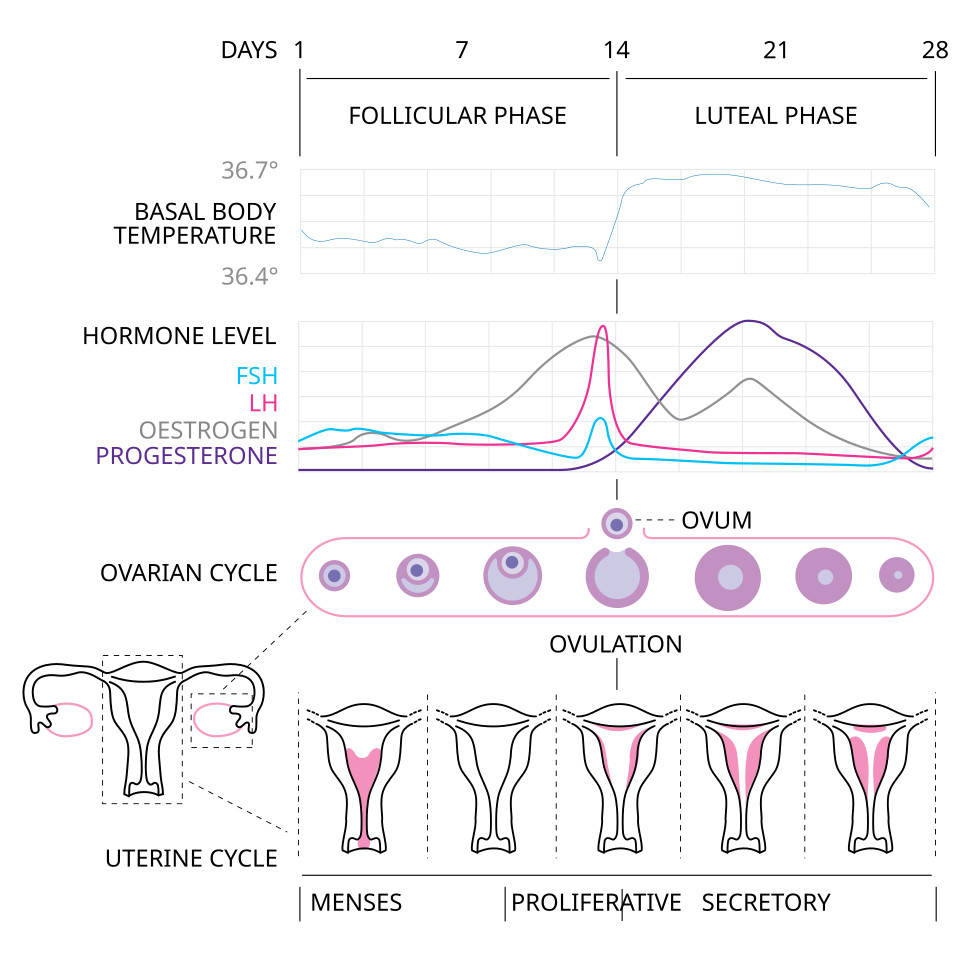
Phase 1: Menstruation (Day 1–4)
- Shedding of endometrial lining due to falling oestrogen and progesterone.
Phase 2: Proliferative (Follicular) Phase (Day 5–13)
Ovarian changes:
- FSH stimulates growth of ovarian follicles.
- One becomes dominant and secretes increasing oestradiol.
Endometrial changes:
- Endometrial proliferation begins.
Hormonal:
- Rising oestradiol (from dominant follicle) leads to LH surge → triggers ovulation.
Cervical mucus:
- Becomes clear and stretchy just before ovulation.
Temperature:
- Slight drop in basal body temp just before ovulation.
Phase 3: Ovulation (Day 14)
- LH surge causes release of oocyte.
Phase 4: Secretory (Luteal) Phase (Day 15–28)
Ovarian changes:
- An ovarian follicle forms into the corpus luteum after the release of the oocyte during ovulation
- The corpus luteum secretes progesterone.
Endometrial changes:
- Endometrium becomes secretory and receptive to implantation.
If no fertilisation occurs:
- Corpus luteum degenerates → progesterone and oestradiol fall → menstruation.
🚫 Amenorrhoea: Background
-
Primary amenorrhoea: No menstruation by:
- 15 years with secondary sexual characteristics
- 13 years if no secondary sexual characteristics
-
Secondary amenorrhoea: The cessation of menstruation in a woman with previous menses for:
- ≥3 months (previously regular cycles)
- ≥6 months if history of oligomenorrhoea
🧬 Causes of Primary Amenorrhoea
With normal secondary sexual characteristics:
- Constitutional delay (family history)
- Endocrine: Thyroid dysfunction, hyperprolactinaemia, Cushing’s
- Androgen insensitivity syndrome
With absent secondary sexual characteristics:
- Turner’s syndrome (45XO)
- Primary ovarian insufficiency
- Hypothalamic dysfunction: stress, weight loss, excessive exercise
🧬 Causes of Secondary Amenorrhoea
With hyperandrogenism:
- PCOS
- Cushing’s syndrome
Without hyperandrogenism:
- Pregnancy/lactation
- Menopause
- Premature ovarian insufficiency
- Hypothalamic dysfunction
- Pituitary: Prolactinoma
- Thyroid dysfunction
🔬 Investigations for Amenorrhoea
Primary Amenorrhoea
Referral to a specialist is recommended. Investigations may include:
- Pelvic US – check uterus/ovaries
- FSH/LH – elevated in ovarian failure - Turner's syndrome
- Prolactin – >1000 → prolactinoma
- TFTs
- Testosterone – raised in androgen insensitivity (can be modestly raised in PCOS)
- Karyotype – e.g. 45XO for Turner’s
Secondary Amenorrhoea
- FSH/LH – high in premature ovarian insufficiency, low in hypothalamic causes
- Prolactin
- TFTs
- Testosterone – for PCOS/hyperandrogenism
- Pelvic USS – >12 follicles or >10cm³ ovarian volume suggests PCOS
🎯 Turner Syndrome
Pathophysiology
- Genetics: 45X,O
- 1 in 2500 females
Clinical Features
- Short stature, webbed neck, wide carrying angle
- Shield chest with wide-spaced nipples
- Primary amenorrhoea (streak ovaries)
- Hypothyroidism common - affects 1/3rd patients (Hashimoto's)

Associated Conditions
- Coarctation of the aorta, VSD
- Horseshoe kidney
- Infertility
Diagnosis and Management
- Karyotyping
- Growth hormone, oestrogen replacement
🌰 Polycystic Ovarian Syndrome (PCOS)
Pathophysiology
- Insulin resistance, hyperinsulinaemia
- Elevated LH and androgens
Clinical Features
- Oligo/amenorrhoea
- Hirsutism, acne
- Acanthosis nigricans, obesity
- Subfertility
Investigations
- Raised LH:FSH ratio
- Mildly raised testosterone
- Low SHBG
- Pelvic USS: ≥12 follicles or ovarian volume >10cm³
Diagnosis: Rotterdam Criteria (2 of 3)
- Oligo/amenorrhoea
- Hyperandrogenism (clinical or biochemical)
- Polycystic ovaries on USS
Management
- COCP for acne/hirsutism
- Weight loss
- Clomifene for fertility
- Metformin may be used
📝 Exam Clues & Clinchers
- Short girl with webbed neck, amenorrhoea, widely spaced nipples → Turner’s syndrome (45XO)
- Oligomenorrhoea + acne + hirsutism + obesity → PCOS
- Amenorrhoea + low FSH/LH + recent stress/weight loss → Hypothalamic dysfunction
- Amenorrhoea + high prolactin → Prolactinoma
- Amenorrhoea + high FSH in woman <40 → Premature ovarian failure
- Primary amenorrhoea + normal breast development + absent uterus → Androgen insensitivity syndrome
