🔑 Key Learning
-
Pregnancy is a hypercoagulable state, increasing VTE risk; D-dimer is not useful in pregnancy
- 1st line treatment: LMWH
- Thyrotoxicosis: propylthiouracil in first trimester, switch to carbimazole for 2nd/3rd trimester.
- Obstetric cholestasis presents with itching, jaundice and raised bile acids; risk of stillbirth increases with bile acid levels
- Acute fatty liver of pregnancy presents with hepatitis and very high ALT; prompt delivery is the treatment
-
Pruritic rashes include
- Polymorphic eruption - pink papules and urticarial plaques, often within stretch marks
- Pemphigoid gestationis - autoimmune blistering
🩸 Venous Thromboembolism in Pregnancy
Pathophysiology
- Increased clotting factors (VII, VIII, X, fibrinogen)
- Decreased protein S
- Venous stasis from IVC compression
Investigations
- Do not use D-dimer - will be raised anyway due to pregnancy
- Suspected DVT: compression duplex ultrasound
-
Suspected PE:
-
If DVT symptoms present → duplex US
- If positive → treat as PE without CTPA (can avoid radiation risk)
-
If no DVT symptoms → CTPA or V/Q after discussion
- CTPA: increased breast cancer risk (~10% increase)
- V/Q: increased childhood cancer risk
-
If DVT symptoms present → duplex US
Management
- First-line: subcutaneous LMWH (e.g. enoxaparin)
🧠 Thyroid Problems in Pregnancy
Thyrotoxicosis
- First trimester: propylthiouracil (due to teratogenicity of carbimazole)
- Second and third trimester: switch to carbimazole (due to hepatotoxicity risk of PTU)
- Aim: keep maternal thyroxine in upper third of normal
Hypothyroidism
- Monitor TSH every trimester and 6–8 weeks post-partum
- Increase levothyroxine dose by ~50% during pregnancy
🧴 Biliary Problems in Pregnancy
Obstetric Cholestasis (Intrahepatic Cholestasis of Pregnancy)
Timing
- Typically third trimester
Diagnosis
- Itching with elevated bile acids ≥19 µmol/L
Clinical Features
- Generalised pruritus (palms and soles)
- Jaundice, dark urine
Complications and Delivery Timing
- Mild (19–39): background stillbirth risk → aim delivery by 40 weeks
- Moderate (40–99): increased risk stillbirth after 38 weeks → delivery at 38–39 weeks
- Severe (≥100): higher risk stillbirth→ consider delivery at 35–36 weeks
Management
- No pharmacological treatments reduce adverse outcomes or bile acid levels
- Ursodeoxycholic acid not routinely offered (removed in most recent guideline)
- Symptom relief: emollients, chlorphenamine
Acute Fatty Liver of Pregnancy (AFLP)
Pathophysiology
- Acute hepatic failure from fat accumulation in hepatocytes
Timing
- Most common in third trimester
Clinical Features
- Abdominal pain, nausea, vomiting, jaundice, ascites
- ALT often > 500
- Thrombocytopenia suggests HELLP instead
Management
- Urgent delivery
🌡️ Rashes in Pregnancy
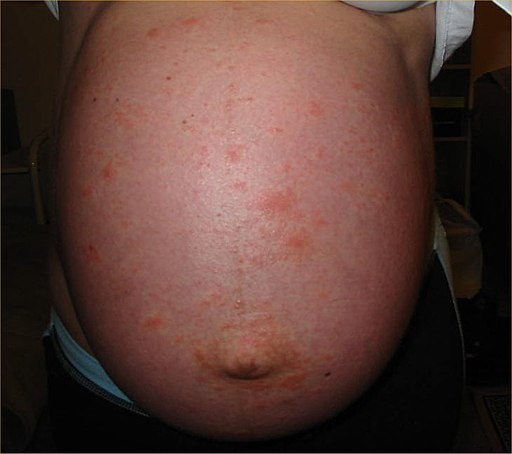
Polymorphic Eruption of Pregnancy (PEP)
Clinical Features
- Also known as pruritic urticarial papules and plaques of pregnancy (PUPPP)
- Intensely itchy, third trimester rash
- Starts in abdominal striae as pink papules → urticarial plaques
- May spread to trunk and limbs
- Resolves after delivery

Management
- Antihistamines
- Topical corticosteroids (oral if severe)
Pemphigoid Gestationis
Pathophysiology
- An autoimmune, blistering rash of pregnancy
- An IgG autoantibody (called PG factor) develops and targets BP-180 proteins within the basement membrane between the epidermis and dermis.
Clinical Features
- Starts around umbilicus in second or third trimester
- Urticarial rash → tense fluid-filled blisters
- May spread to trunk, limbs, buttocks
Management
- Topical corticosteroids if mild
- Systemic corticosteroids if severe
📝 Exam Clues & Clinchers
- Pregnancy + leg swelling → suspect DVT → duplex US
- Suspected PE + DVT symptoms → US first; if positive, no need to do CTPA
- Hyperthyroid in pregnancy → PTU in first trimester, switch to carbimazole later
- Itchy palms/soles + raised bile acids in late pregnancy → obstetric cholestasis
- ALT > 500 + third trimester + acute hepatitis signs → acute fatty liver
- Umbilical-centred itchy blistering rash → think pemphigoid gestationis
- Very itchy rash in striae, no blisters → think polymorphic eruption
🔗 Useful Links and References
-
RCOG Green-top Guideline 37b: Thromboembolic Disease in Pregnancy
https://www.rcog.org.uk/media/wj2lpco5/gtg-37b-1.pdf - RCOG Green-top Guideline 43: Intrahepatic Cholestasis of Pregnancy https://obgyn.onlinelibrary.wi...
