🔑 Key Learning
-
Dysmenorrhoea = menstruation-related abdominal pain.
-
Primary dysmenorrhoea = no underlying pelvic pathology (common in adolescents).
- First-line management is NSAIDs; COCP can be considered if contraception is acceptable.
-
Secondary dysmenorrhoea = associated with pathology (endometriosis, adenomyosis, PID, fibroids).
- Always exclude pathology before diagnosing primary dysmenorrhoea.
🧬 Pathophysiology
-
Primary dysmenorrhoea: excessive prostaglandin release causing painful uterine contractions.
-
Secondary dysmenorrhoea: pain due to underlying structural or inflammatory pelvic pathology.
👀 Clinical Features
Primary Dysmenorrhoea
-
Cramping lower abdominal pain starting just before menstruation and lasting 2–3 days.
-
Typically begins around 6 months after menarche.
-
No associated gynaecological symptoms.
Secondary Dysmenorrhoea
-
Painful periods previously absent or now different in character.
-
Pain starts 3–4 days before menstruation and may continue after.
-
Other gynaecological symptoms: vaginal discharge, bleeding, dyspareunia, menorrhagia.
-
Suggestive of endometriosis, adenomyosis, PID, fibroids.
🧪 Investigations
-
Pelvic ultrasound to identify fibroids, adenomyosis, endometriosis.
-
High vaginal/endocervical swabs to exclude STIs.
-
Pregnancy test to exclude pregnancy-related causes.
💊 Management of Primary Dysmenorrhoea
Step 1
-
1st line: NSAIDs (ibuprofen, naproxen, mefenamic acid).
- Alternative 1st line if not trying to conceive: Hormonal contraception (e.g. COCP) for 3–6 months if contraception is acceptable.
-
Add paracetamol if required, or use paracetamol alone if NSAIDs contraindicated.
- If treatment is ineffective: Combine NSAID + hormonal contraception
Step 2
-
Combination of NSAID (or paracetamol) + COCP.
💥 Management of Secondary Dysmenorrhoea
-
Management depends on underlying cause (refer to specific condition notes).
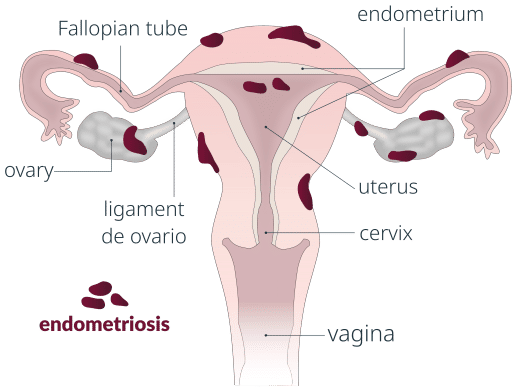
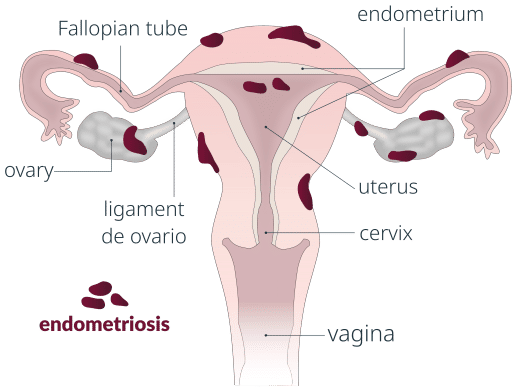
🩸 Endometriosis
🧬 Pathophysiology
-
Endometrium-like tissue outside the uterine cavity (commonly pelvis).
-
Tissue bleeds, causing inflammation and scar tissue formation in response to menstrual cycle hormones.
 Endometriosis. Vega asensio, CC BY-SA 4.0, via Wikimedia Commons
Endometriosis. Vega asensio, CC BY-SA 4.0, via Wikimedia Commons
👀 Clinical Features
-
Secondary dysmenorrhoea.
-
Chronic pelvic pain.
-
Deep dyspareunia.
-
Subfertility or infertility.
-
Bowel symptoms (e.g. pain on defecation).
🧪 Investigations
-
Laparoscopy is gold standard for definitive diagnosis (classic finding: ‘chocolate cysts’ or endometriomas).
-
TVUS/TAUS may be supportive.
💊 Management
-
Refer for specialist assessment.
-
Pain management:
- Trial of paracetamol and/or NSAID.
-
Hormonal therapy: COCP, POP, implant, Mirena IUS, or depot injections.
-
Surgery in secondary care if medical management fails.
🩺 Adenomyosis
🧬 Pathophysiology
-
Extension of endometrial tissue into uterine myometrium.
👀 Clinical Features
-
Menorrhagia.
-
Irregular periods.
-
Dysmenorrhoea.
🧪 Diagnosis
-
MRI pelvis: enlarged uterus with thickened myometrium.
🔗 Useful Links and References
NICE CKS. Dysmenorrhoea [Last revised October 2023].