🔑 Key Learning
- Caused by compression of a cervical nerve root, typically C7 or C6.
- Presents with neck pain, radicular arm pain, and dermatomal sensory or motor symptoms.
- Diagnosis is clinical, confirmed by MRI if symptoms persist > 4–6 weeks or if there is objective neurology.
- Initial management is conservative unless red flags or severe neurology are present.
🧬 Pathophysiology
- Nerve root compression causes radicular pain and neurology along the affected dermatome.
-
Most common causes:
- Degenerative disc disease
- Cervical disc herniation
- Cervical spondylosis
-
Most frequently affected nerve roots:
- C7 (most common)
- C6 (next most common)
👀 Clinical Features
Symptoms
- Neck pain
- Radiating arm pain – often burning or shooting, following a dermatomal distribution
- Night pain
- Sensory symptoms – paraesthesia, numbness in a dermatomal pattern
- Motor symptoms – weakness in corresponding myotomes
🧪 Examination
General
- Restricted neck movement
-
Spurling's test positive:
- Neck extension, lateral rotation, and axial compression reproduce pain or neurology
- Suggestive of radiculopathy
C6 Nerve Root
- Motor: Weakness in elbow flexion and wrist extension
- Reflexes: Decreased biceps and supinator reflex
- Sensation: Lateral forearm, thumb, and index finger
C7 Nerve Root
- Motor: Weakness in elbow extension, wrist flexion, finger extension
- Reflex: Decreased triceps reflex
- Sensation: Middle finger
🧪 Investigations
- Clinical diagnosis if < 4–6 weeks and no red flags
-
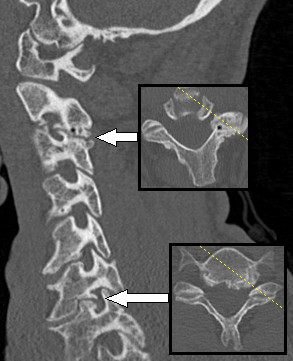
MRI cervical spine:
- If symptoms persist > 4–6 weeks
- If neurological deficit is present
- May show disc herniation, osteophytes, or foraminal stenosis
💊 Management
Immediate referral
-
If red flags or progressive neurological signs
- Refer urgently for spinal surgical opinion
Conservative
-
If symptoms < 4–6 weeks and no neurological deficit:
- Simple analgesia (e.g. paracetamol, NSAIDs)
- Consider neuropathic analgesia (e.g. amitriptyline, gabapentin)
- Physiotherapy
Further Management
-
If symptoms > 4–6 weeks or objective neurology on exam:
- Perform MRI
-
Refer for specialist management
- Consider spinal injections
-
Consider surgery (e.g. decompression, discectomy) if:
- Progressive weakness
- Persistent pain despite 6–12 weeks of conservative therapy
📝 Exam Clues & Clinchers
- Neck pain + radiating arm pain + sensory loss → think cervical radiculopathy
- C7 = triceps weakness, middle finger sensory loss
- Spurling’s test helps reproduce symptoms
- MRI is the investigation of choice if symptoms persist
| Feature | Cervical Radiculopathy | Cervical Myelopathy |
|---|---|---|
| 🧬 Pathophysiology | Compression of a nerve root | Compression of the spinal cord itself |
| 🔍 Anatomy involved | Exiting cervical nerve root (e.g. C6, C7) | Cervical spinal cord (central canal stenosis) |
| 👤 Typical patient | Younger adults with disc herniation, or spondylosis | Older adults with degenerative cervical stenosis |
| ⚡ Symptoms | Unilateral pain, tingling, numbness in a dermatome | Bilateral symptoms, clumsy hands, gait disturbance |
| 💪 Motor findings | Weakness in specific myotome | Weakness + spasticity below the level of compression |
| 🦶 Reflexes | Decreased reflexes at affected level (LMN signs) | Hyperreflexia, positive Babinski, Hoffmann (UMN) |
| 🧪 Special tests | Positive Spurling’s test | Positive Lhermitte’s sign, gait abnormalities |
| 🔬 Diagnosis | MRI cervical spine (nerve root compression) | MRI cervical spine (cord compression, signal change) |
| 💊 Management | Often conservative; surgery if progressive | Usually requires surgical decompression |
🔗 Useful Links and References
- NICE CKS – Cervical Radiculopathy (2023)
